Is it "Bad Periods" or Endometriosis?
- Endometriosis occurs when tissue like uterine lining grows outside the uterus.
- Symptoms go beyond cramps to fatigue, digestive issues and mental health.
- Early care helps manage symptoms and preserve quality of life.
Sub-Heading
Painful periods are often brushed off as ‘just part of being a woman.’ What if the pain is not normal? What if it is your body trying to tell you something more?
According to the WHO, endometriosis affects an estimated 1 in 10 women, yet it can take years to be diagnosed. This delay is not just about missed medical appointments; it is also about the way we have been taught to minimise and normalise pain. In this article, we will explore how to tell the difference between a tough period and a potential underlying condition, so that you can seek help sooner rather than later.
Understanding Endometriosis
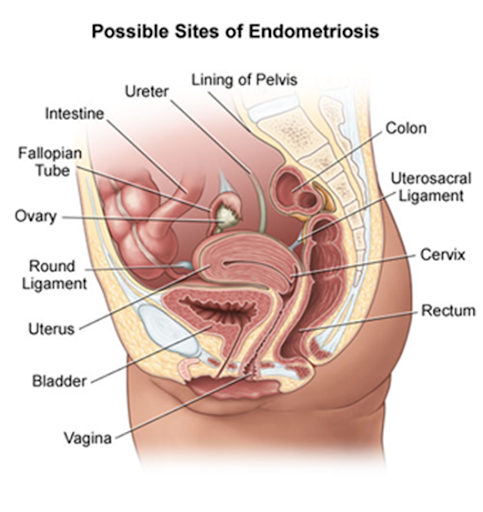
The inner lining of the uterus is lined with a tissue called endometrium. Every menstrual cycle the uterus grows a new endometrium to prepare for a fertilized egg. Endometriosis occurs when the endometrial tissue grows outside the uterus.
These misplaced growths can attach to organs within the pelvic cavity. They can trigger inflammation, lead to scar tissue formation and cause fluid-filled cysts. Endometriosis is a chronic condition that may appear as early as a person’s first period and persist until menopause.
While its exact cause is still unknown, various treatments can help reduce symptoms and maintain a good quality of life.
Where can Endometriosis occur?
Endometriosis is not limited to one location. It can grow:
- On the surface of the pelvic cavity lining
- Fallopian tubes
- Ligaments around the uterus
- Space between the uterus and rectum or bowel
- Outside the surface of uterus
More rarely, it can also grow on and around the:
- Bladder
- Cervix
- Intestines
- Rectum
- Stomach
- Vagina or vulva
Recognising the Symptoms
Symptoms can range from mild to debilitating and some people experience none at all. Common signs include:
- Severe period pain that disrupts daily activities
- Pain during or after sex
- Painful urination or bowel movements, especially during periods
- Heavy or irregular menstrual bleeding
- Chronic pelvic pain, bloating or nausea
- Fatigue and low energy
- Difficulty getting pregnant
- Emotional distress, anxiety or depression linked to chronic pain
Why is it Often Missed?
Endometriosis is known for being hard to diagnose. Its symptoms overlap with other conditions like irritable bowel syndrome or pelvic inflammatory disease. On top of that, society often normalises menstrual pain, leading many to dismiss symptoms for years before seeking help. As a result, diagnosis can take an average of 7–10 years.
Who is at Higher Risk?
While endometriosis can affect anyone with a menstrual cycle, certain factors may increase risk:
- Starting periods at an early age
- Short menstrual cycles (less than 27 days)
- Heavy or prolonged periods
- A family history of endometriosis
- Low body mass index
How is it Diagnosed?
There is no simple blood test for endometriosis. Diagnosis usually involves:
- Reviewing symptoms and menstrual history
- Pelvic exams and ultrasound imaging
- MRI for detailed pelvic views
- Laparoscopy (a minor surgical procedure) for definitive diagnosis
Managing the Condition
While there is no cure as of now, treatment for endometriosis aims to reduce symptoms and improve quality of life. Options include:
- Pain relief Medication
- Hormone therapy to slow tissue growth
- Laparoscopic surgery to remove growths and scar tissue
- Fertility support for those trying to conceive
- Lifestyle changes such as exercise, dietary adjustments and stress management

Conclusion
Undiagnosed endometriosis can mean years of unnecessary suffering. Knowing what is normal for your body and what is not is key. If pain is interfering with your life, keep a symptom diary and speak to a healthcare professional. The earlier it is caught, the sooner it can be managed.
Author