Your Guide: Everything About HPV Vaccines
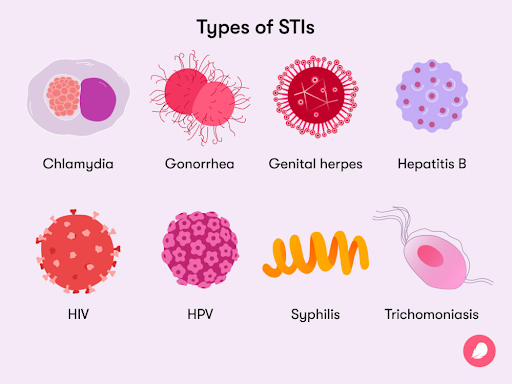
Vaccination plays a crucial role in preventing sexually transmitted infections (STIs) by protecting against specific pathogens that can be transmitted through sexual contact. Human papillomavirus, a Sexually Transmitted Infection, can be prevented via its vaccination i.e. HPV Vaccine. It can help significantly reduce the overall transmission of the infection within the community and reduce the risk of cancer-related deaths.
If you are someone who is sexually active and wants to know more about HPV, then this guide is here to help you out!
WHAT IS HPV?
The Human papillomavirus (HPV) is a form of STI and belongs to the group of viruses. There are more than 200 types of HPV and about 40 of them are spread through direct sexual contact with someone who has the virus. They can also spread through other intimate, skin-to-skin contact. Some of these types can cause cancer.
Its symptoms include
- Warts on different parts of your body. Around your genitals, anus, mouth, or throat. – for low-risk HPV Infection
- High-risk HPV infection lasts many years and causes cell changes, which can have symptoms depending on which body part is infected. They are the most significant source of cancers, like cervical, anal, vaginal, penile or vulvar cancer.
But how to get diagnosed?
- If your symptoms include warts, then your healthcare provider will be able to diagnose them by looking at them.
- For cervical cancer specifically, women can get cervical cancer screening tests done, like, a Pap test, HPV test, or both.
How deadly is HPV?
Interestingly, nearly all sexually active people are infected with HPV within months to a few years of becoming sexually active. Most HPV infections don’t cause cancer. Our immune system usually clears most of HPV infections. Only about 1% of High-risk HPV infections that persist can cause cancer.
ABOUT HPV VACCINE
Like other immunizations that guard against viral infection, HPV vaccines stimulate the body to produce antibodies that, in future encounters with HPV, bind to the virus and prevent it from infecting cells. The current HPV vaccines are based on virus-like particles (VLPs) that are formed by HPV surface components. VLPs are not infectious because they lack the virus’s DNA.
The vaccines do not prevent other sexually transmitted diseases, nor do they treat existing HPV infections or HPV-caused diseases and work the best, when taken before first sexual intercourse.

AVAILABILITY IN INDIA
Types of HPV Vaccines available in India:
- Gardasil – Quadrivalent vaccine, licensed for use since June 2006, by the FDA & since 2008 in India. It targets four strains of human papillomavirus (HPV).
- Gardasil – 9 – Nonvalent vaccine, licensed for use in India since 2018 prevents infection with the nine HPV types.
- Cervavac – Quadrivalent It targets four strains of human papillomavirus (HPV) – HPV-6, 11, 16, and 18. This is India’s first indigenous vaccine available in the market since January 2023. India’s first homegrown HPV vaccine by Serum Institute of India can be a game changer as it will be more affordable and accessible.
But what will this cost you?
The Serum Institute’s made-in-India vaccine against cervical cancer, CERVAVAC, is available in the market at an MRP of Rs 2,000 per vial of two doses, as last updated on February 2023. This is in stark contrast to the average cost of dosing for all international vaccines which ranges from INR 3000 to 10000 per dose.
There are initiatives by the Serum Institute, to make the vaccine available under the cost bracket of 200-400 Rupees per dose.
Dosage Recommendations:
The preferred target age group is 9-14 years. Two doses: 0 & 6 months (the second dose may be given at 5-15 months)
- Catch-up vaccination (15-26 years) Three doses: 0, 1, 6 months (Bivalent, No longer available in India) 0, 2, 6 months (Quadrivalent & Nonavalent)
- Older age groups (27-45 years) Three doses: 0, 1, 6 months (Bivalent) & 0, 2, 6 months (Quadrivalent & Nonavalent). Women aged > 26 years who have been sexually active should be counselled regarding reduced efficacy in older age groups and the importance of screening.
CONCLUSION
Most HPV infections go away on their own and don’t cause cancer. But sometimes the infections last longer. When a high-risk HPV infection lasts for many years, it can lead to cell changes. If these changes are not treated, they may worsen and become cancer.
It’s important to note that not all STIs have vaccines available, (only two as of now) and vaccination is just one part of a comprehensive approach to STI prevention. Safe sexual practices, regular testing, and education about STIs are also crucial components of preventing the spread of these infections. Individuals should consult with healthcare providers to determine which STI vaccines are appropriate for them based on their age, risk factors, and overall health.
Author