Your A-Z Guide to Sexually Transmitted Diseases During Pregnancy
Sexually transmitted infections, also known as sexually transmitted diseases, are infections that are disseminated through sexual interaction involving the mouth, anus, or vagina and are generally caused by bacteria, viruses, or parasites.
According to research by the World Health Organisation, more than 1 million sexually transmitted infections are acquired every day worldwide, making it impossible to list them all.
But some of the most common STIs are listed as follows:
- Chlamydia is a common sexually transmitted infection (STI) caused by bacteria and is generally treatable and curable, but if left untreated, it can cause severe complications as well as permanent damage to the reproductive organs.
- Genital Herpes: Herpes simplex is a virus that causes skin infections and is lifelong. It causes painful or itchy sores and blisters. The virus typically doesn’t cause severe problems but can be very dangerous for infants and people with weakened immune systems.
- Gonorrhea is a common sexually transmitted infection (STI) caused by a bacteria called Neisseria gonorrhoeae. It also spreads through sexual fluids, including vaginal fluid and semen. One can get gonorrhoea from intercourse, anal sex, oral sex, and sharing sex toys with an infected partner.
- Hepatitis B is a viral infection that affects the liver. It causes inflammation in the liver tissues and generally begins as an acute infection that’s usually short-lived. But for some people, it turns into a lifelong chronic infection.
- HIV stands for human immunodeficiency virus. HIV infects and destroys cells in the immune system, making it hard to fight off other diseases and can lead to Acquired Immunodeficiency Syndrome (AIDS) which is lethal to the health.
- Syphilis is a sexually transmitted infection (STI) that is treatable with medication. Without treatment, syphilis causes serious health problems.
It can permanently damage the heart, brain, muscles, bones, and eyes.
What are the common symptoms of an STI?
Most STIs are ‘silent’ and therefore have no visible symptoms, so one might not know if they are infected. If a person is sexually active, regularly testing themselves is the best option to know whether or not they are affected by an STI or not.
Bumps, blisters, or warts in the mouth, anus, or vagina; swelling or redness near the male or female reproductive organ; as well as skin rashes and painful urination, represent the most common symptoms.
Regular bleeding apart from the monthly period cycle, sudden weight loss, jaundice, loose stools, and night sweats, along with vaginal discharge with an unbearably foul smell as well as itching near it, are some of the other common symptoms.
How to avoid the risk of getting an STI while trying to conceive a baby?
If one is sexually active, there are generally two scenarios:
- A) Trying to conceive while avoiding STIs
As previously stated, the majority of STIs are asymptomatic. The only way to avoid those unpleasant STIs is to be in a long-term, mutually monogamous relationship with a partner who has been tested and has a negative result.
Be aware of the signs and symptoms of an STI, visit a healthcare provider, and learn about them. The more you are informed about STIs, the better you can protect yourself, your partner, and the baby.
- B) Not Attempting to Conceive
Using latex or non-latex condoms is the most effective way to avoid not only unwanted pregnancies but also potentially fatal STIs.
Even though condoms are not 100% effective in preventing unwanted pregnancy, they remain one of the most popular and effective forms of contraception. They are also one of the most reliable contraceptives for preventing sexually transmitted infections (STIs) and urinary tract infections (UTIs).
Apart from this using a dental dam and regularly getting tested is another way to avoid those STIs
Can a pregnant woman contract an STD or STI? Is it advisable to get examined and treated for the same when bearing a child?
Indeed, the answer is “yes.”
Pregnant women can become infected with sexually transmitted diseases or infections, as pregnancy does not provide women or their babies with any additional protection against STIs
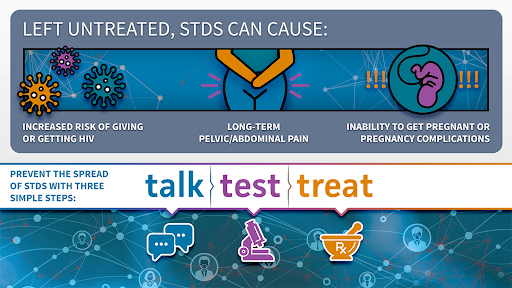
Detecting, testing, and treating pregnant women for STDs is crucial for preventing any serious health complications for not only the mother but also the development of her baby. Another critical step is to see a health care provider and have an open and transparent conversation about the symptoms as well as the condition and any high-risk sexual behaviour that one might be engaging in.
Even if the person has already been tested, it is recommended that they get themselves tested again once they are pregnant with a child. The “2015 STD Treatment Guidelines from the Centres for Disease Control and Prevention” advocate screening pregnant women for STDs, which the health care practitioner ought to execute at all costs.
The table below incorporates these guidelines.
Sexually Transmitted Infection | CDC Recommendations |
Chlamydia | First prenatal visit: Screen all pregnant women who are at an increased risk for the infection. Third trimester: Rescreen if they are at a continued high risk. Risk Factors: •New or multiple sex partners. •Being Sexually active with concurrent partners. •Partner who has a sexually transmitted disease (STD) NOTE: Pregnant women who identify with chlamydial infection should have a cure test three to four weeks after the end of their treatment and should be retested within three months. |
Gonorrhea | First prenatal visit: Screen all pregnant women who are at increased risk for gonorrhoea at the first prenatal visit. Third trimester: Rescreen for women at continued high risk. Risk factors: •Living in a high-morbidity area •Previous infected with an STI •New or multiple sex partners •Inconsistent use of condoms while engaging with people who are not in mutually monogamous relationships •Exchanging sex for money or drugs |
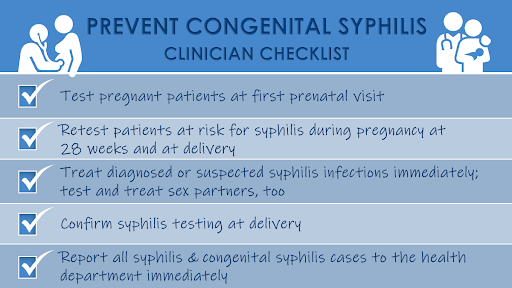
Syphilis | First prenatal visit: Screen all pregnant women. Third trimester (28 weeks and at delivery): Rescreen •Women who are at risk for syphilis during pregnancy (e.g., misuses drugs; has had another STI during pregnancy; or has had multiple sex partners, a new partner, or a partner with an STI) •Women who live in areas with high numbers of syphilis cases •Women who were not previously tested, or had a positive test in the first trimester. |
Conclusion
Pregnant couples who are tested negative for STDs before trying to get pregnant provided themselves with a healthier start to their beautiful journey of pregnancy.
It is important to note that STDs don’t just appear from nowhere; they have to be passed from one person to another. Thus, they can be passed from one partner to another and from mother to child, which can be very dangerous for their initial development as well as lead to complications during the pregnancy and at the time of birth.
However, this doesn’t mean that one cannot have kids if they are infected with an STI, as most sexually transmitted diseases and infections are certainly curable and treatable.
However visiting a health care provider, getting the right guidance, treatment, and medications, and waiting until both partners have tested negative for an STI before planning to start a family is a must.
Author

Muskan Rawat
Author
-
Muskan (she/her) is a 21-year-old ambivert girl with a major in history from the University of Delhi. She is a published writer and a feminist who believes in equity among all and is continuously thriving to make an impact for the right cause
View all posts

1 thought on “Your A-Z Guide to Sexually Transmitted Diseases During Pregnancy”
Get rid of the Hsv………………………