Bleeding To Birth: Understanding Postpartum Haemorrhage
- PPH is the loss of 1000 ml of blood post childbirth.
- Uterine Atony is the leading cause of PPH.
- PPH can cause long-term cardiovascular problems.
The World Health Organisation defined Postpartum Haemorrhage or PPH as the loss of 500 ml or more of blood of a pregnant person within 24 hours after childbirth. This may be followed by a range of severe medical issues including, negative overall memory of the birth of their child, as reported in two-third of the cases. PPH also causes psychological trauma leading to fear of conceiving again and this is amidst the long-term cardiovascular risks. While Neonatal, Fetal and Postpartum Care and strategies for emergency intervention is necessitated, it is important to first understand PPH and its long-term effects.
Data, Definition and Analysis
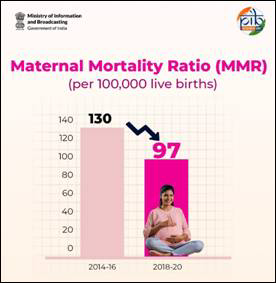
Occurring in 1-3% of all deliveries worldwide, PPH is a leading cause of maternal mortality and morbidity. Globally, there are 14 million cases of PPH every year. It accounts for 8% of maternal deaths in developing countries and 20% in developed countries. In India, PPH occurs in 2-4% of vaginal deliveries and it is responsible for 19.9% of maternal deaths. Uterine contractions and coagulation, that is the turning of blood to a thicker liquid form and the ultimate formation of a clot, increases dramatically leading to severe complications if left untreated.
The traditional definition of PPH was a loss of more than 500 mL of estimated blood loss in a vaginal delivery or more than 1000 mL of estimated blood loss during Cesarean delivery. But in 2017, the parameters were redefined by the American College of Obstetrics and Gynaecology as the cumulative blood loss of more than 1000 mL with signs and symptoms of hypovolemia within 24 hours of the birth process, regardless of the mode of delivery. This is however debated by scientists as 500 ml is considered as abnormal enough and demanding severe attention.
PPH is classified on the basis of the onset of its symptoms and it is as follows:
- Primary PPH: A hemorrhage that occurs between the third stage of labor (that is, delivery of the placenta) and 24 hours after delivery.
- Secondary PPH: Occurs more than 24 hours after delivery and lasts up to 12 weeks postpartum.
Causes of PPH are summarised as the “4 Ts” and these are tone, trauma, tissue and thrombin. These signify uterine atony, uterine rupture or lacerations, retained placenta or clots and coagulation deficiency, respectively. Uterine Atony is alone responsible for 70% of the cases of PPH. These require a multidisciplinary approach emphasizing on blood loss assessment, fluid replacement, and source control.
Treatment and Management of PPH
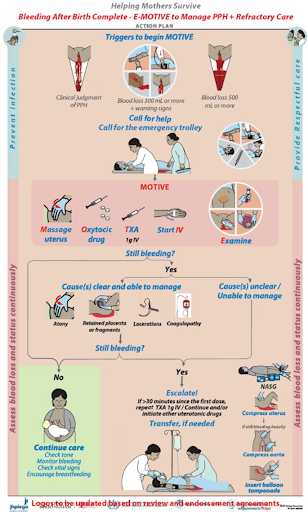
PPH intervention focuses on the patient’s resuscitation while identifying and treating the underlying causes. Maintaining the patient’s steady blood flow is cardinal to ensure continued blood supply to vital organs.
Because Uterine Atony is a leading cause of PPH, it is advised to assess whether the uterus is soft and without physiologic contraction following delivery. In the instance of excessive bleeding, removal of clots and bimanual massage should be prioritised by the physician. After this, an elaborative medical procedure is followed which is best left to the understanding of medical professionals.
Patients who have had PPH in a previous delivery are at a higher risk of having it subsequently, and hence, implementation of standardized PPH protocols and interprofessional simulation training can help improve patient outcomes.
Prioritising Prevention over Cure
Research by the National Library of Medicine found that increased efforts to enhance coordination among healthcare team members in response to PPH have contributed to reduced maternal morbidity. Rapid identification of the cause, controlling the bleeding and initiating treatment is the priority. However, this is not possible without a cohesive interprofessional team that comprises physicians, technicians, nurses, pharmacists, laboratory personnel, and labor and delivery nurses who effectively communicate and coordinate to optimize patient-centred care.
In a country, like India, where postpartum monitoring is limited typically to the first six weeks, awareness about the cardiovascular risk posed by PPH is vital. The structural health gaps in India often results in iron deficient, anaemic and malnourished persons becoming pregnant, which makes them vulnerable to other complications such as anemia-induced hypertension
While the primary focus should be reducing PPH, detection and treatment cannot be ignored.
The E-MOTIVE clinical trial includes a calibrated blood-collection drapes and a rapid treatment bundle (including uterine massage, oxytocics, tranexamic acids, IV fluids, valuation and escalation protocols) that has proven to reduce adverse PPH outcomes by 60%, as per a Lancet Health study.
Call to Action
Knowledge is Power and without a general knowledge about cases like PPH, no national strategy or institutional framework will be effective in preventing mortality. This is why, Comprehensive Sexuality Education (CSE), as a progressive curriculum introduced at the elementary level of education and carried on to every new step of life is emphasised.
Institutionally, the need of the hour is a robust response system that focuses on training ASHA workers and traditional birth attendants (TBA) in recognising danger signs, and carrying out early interventions to cater to the larger population of India. Other than this, ensuring the availability of life-saving drugs, strengthening antenatal care, and promoting institutional deliveries are all critical steps to ensure long-term health care.
Author


1 thought on “Bleeding to Birth: Understanding Postpartum Haemorrhage”
Wow, what an article raising an issue from past, present and coming future. Well researched and thoughtful to think and discuss issues which is happening daily, hourly and every minutes or seconds on this earth buy taken as quite normal. Mar Gayi Bechari, Bachhe ka kya hoga, koi nahi, baap ne Dusari shadi kar li. What a traumatic experience for a Mother on this Mother earth!!!