Everything You Should Know About Urinary Incontinence
How about you involuntarily urinate all the time? The question here is, ‘Is urination a voluntary process in the first place?’ YES and NO! Urination in infants is involuntary. However, it becomes partially voluntary in adults with practice and observation. Certain brainstem neurons that develop over time allow adult humans to voluntarily control their urination “before the bladder reaches its capacity”. This is called “continence”.
After the capacity of the bladder is outreached, involuntary micturition (voiding of urine) is bound to follow. However, this voluntary control of urine is often lost due to varied causes leading to “Incontinence”.
Athletic Urinary Inconsistence and its risky sections :
Urinary incontinence can be defined as urinary incontinence (also known as an overloaded bladder) as the “loss of bladder control, varying from a slight loss of urine after sneezing, coughing or laughing, to complete inability to control urination”. While browsing through the most standard sites, there was this ethically substandard content calling this problem “embarrassing “. Well, humble opinions of a genuine mind consider embarrassment pertaining to a problem as mere impaired social perception of the problem. Biology is beautiful enough wherein diseases are painful but never embarrassing because nature accounts for all of it.
Urinary incontinence is found to be quite common in females and the elderly.

Warning signs or lower urinary tract symptoms:
Lower urinary tract symptoms (LUTS): The lower urinary tract includes the bladder and the tube that urine passes through as it leaves the body (urethra).
Lower urinary tract symptoms (LUTS) are common as people get older.
They can include:
- problems with storing urine, such as an urgent or frequent need to pass urine or feeling like you need to go again straight after you’ve just been
- problems with passing urine, such as a slow stream of urine, straining to pass urine, or stopping and starting as you pass urine.
- problems after you’ve passed urine, such as feeling that you’ve not completely emptied your bladder or passing a few drops of urine after you think you’ve finished

Causes and Classification:
The causes of urinary incontinence remain unclear because distinguishing the loss of voluntary control of urination from that of involuntary control needs the assessment of neuronal control of urination in awake and actively functioning live subjects. So, the root causes may not be clearly studied. However, accompanying or superficial causes include:
- urinary tract infections
- vaginal infections or irritation
- Constipation
- overactive bladder muscles
- damage to nerves that control urination as seen in multiple sclerosis or Parkinson’s disease
- arthritis( which makes it difficult to get to the bathroom on time)
- pelvic organ prolapse and most importantly “pelvic floor injury”(which leads to weekend pelvic muscles). A common type of urinary incontinence arising due to pelvic floor injury in female athletes is athletic urinary incontinence which can severely affect the performance of female athletes.
Following are a few types of urinary incontinence based on differences in symptoms:
- Stress incontinence: Urine leaks when you exert pressure on your bladder by coughing, sneezing, laughing, exercising, or lifting something heavy.
- Urge incontinence: You have a sudden, intense urge to urinate followed by an involuntary loss of urine. You may need to urinate often, including throughout the night. Urge incontinence may be caused by a minor condition, such as infection, or a more severe condition such as a neurological disorder or diabetes.
- Overflow incontinence: You experience frequent or constant dribbling of urine due to a bladder that doesn’t empty completely.
- Functional incontinence: A physical or mental impairment keeps you from making it to the toilet in time. For example, if you have severe arthritis, you may not be able to unbutton your pants quickly enough.
- Mixed incontinence: You experience more than one type of urinary incontinence — most often this refers to a combination of stress incontinence and urges incontinence.

How do you confirm you have urinary incontinence?
Following are the diagnostic procedures found helpful in detecting urinary incontinence:
- Urinalysis: A sample of your urine is checked for signs of infection, traces of blood, or other abnormalities.
- Bladder diary: For several days you record how much you drink when you urinate, the amount of urine you produce, whether you had an urge to urinate, and the number of incontinence episodes.
- Postvoid residual measurement: You’re asked to urinate (void) into a container that measures urine output. Then your doctor checks the amount of leftover urine in your bladder using a catheter or ultrasound test. A large amount of leftover urine in your bladder may mean that you have an obstruction in your urinary tract or a problem with your bladder nerves or muscles.
If further information is needed, your doctor may recommend more-involved tests, such as urodynamic testing and pelvic ultrasound. These tests are usually done if you’re considering surgery.
Treatment:
Vaginal estrogen cream may help relieve urge or stress incontinence. A low dose of estrogen cream is applied directly to the vaginal walls and urethral tissue.
Medications:
Medications that come in a pill, liquid, or patch may be prescribed to help with bladder control problems. However, some medications for overactive bladder have been associated with a higher risk of cognitive decline in adults over age 65. Talk with your doctor about what drugs, if any, would work best for you.
Medications commonly used to treat incontinence include:
- Anticholinergics: These medications can calm an overactive bladder and may be helpful for urge incontinence. Examples include oxybutynin (Ditropan XL), tolterodine (Detrol), darifenacin (Enablex), fesoterodine (Toviaz), solifenacin (Vesicare), and trospium chloride.
- Mirabegron (Myrbetriq): Used to treat urge incontinence, this medication relaxes the bladder muscle and can increase the amount of urine your bladder can hold. It may also increase the amount you are able to urinate at one time, helping to empty your bladder more completely.
- Alpha-blockers: In men who have urge incontinence or overflow incontinence, these medications relax bladder neck muscles and muscle fibers in the prostate and make it easier to empty the bladder. Examples include tamsulosin (Flomax), alfuzosin (Uroxatral), silodosin (Rapaflo), and doxazosin (Cardura).
- Topical estrogen: Applying low-dose, topical estrogen in the form of a vaginal cream, ring, or patch may help tone and rejuvenate tissues in the urethra and vaginal areas.
Surgery to treat Urinary Incontinence:
Surgery can sometimes improve or cure incontinence if it is caused by a change in the position of the bladder or blockage due to an enlarged prostate.
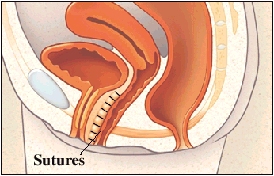
- Sling procedures: Synthetic material (mesh) or strips of your body’s tissue are used to create a pelvic sling underneath your urethra and the area of thickened muscle where the bladder connects to the urethra (bladder neck). The sling helps keep the urethra closed, especially when you cough or sneeze. This procedure is used to treat stress incontinence.
- Bladder neck suspension: This procedure is designed to provide support to your urethra and bladder neck — an area of thickened muscle where the bladder connects to the urethra. It involves an abdominal incision, so it’s done during general or spinal anesthesia.
- Prolapse surgery: In women who have pelvic organ prolapse and mixed incontinence, surgery may include a combination of a sling procedure and prolapse surgery. Repair of pelvic organ prolapse alone does not routinely improve urinary incontinence symptoms.
- Artificial urinary sphincter: A small, fluid-filled ring is implanted around the bladder neck to keep the urinary sphincter shut until there’s a need to urinate. To urinate, you press a valve implanted under your skin that causes the ring to deflate and allows urine from your bladder to flow.

Medical Devices to cure Urinary Incontinence:
- Urethral insert: A small, tampon-like disposable device inserted into the urethra before a specific activity, such as tennis, that can trigger incontinence. The insert acts as a plug to prevent leakage and is removed before urination.
- Pessary: A flexible silicone ring that you insert into your vagina and wear all day. The device is also used in women with vaginal prolapse. The pessary helps support the urethra, to prevent urine leakage.
Electrical stimulation:
Electrodes are temporarily inserted into your rectum or vagina to stimulate and strengthen pelvic floor muscles. Gentle electrical stimulation can be effective for stress incontinence and urge incontinence, but you may need multiple treatments over several months.

Behavioral techniques:
- Bladder training: to delay urination after you get the urge to go. You may start by trying to hold off for 10 minutes every time you feel the urge to urinate. The goal is to lengthen the time between trips to the toilet until you’re urinating only every 2.5 to 3.5 hours.
- Double voiding: To help you learn to empty your bladder more completely to avoid overflow incontinence. Double voiding means urinating, then waiting a few minutes and trying again.
- Scheduled toilet trips: To urinate every two to four hours rather than waiting for the need to go.
- Fluid and diet management: To regain control of your bladder. You may need to cut back on or avoid alcohol, caffeine, or acidic foods. Reducing liquid consumption, losing weight, or increasing physical activity also can ease the problem.

Absorbent pads and catheters:
If medical treatments can’t eliminate your incontinence, you can try products that help ease the discomfort and inconvenience of leaking urine:
- Pads and protective garments: Most products are no bulkier than regular underwear and can be easily worn under everyday clothing. Men who have problems with dribbles of urine can use a drip collector — a small pocket of absorbent padding that’s worn over the penis and held in place by close-fitting underwear.
- Catheter: If you’re incontinent because your bladder doesn’t empty properly, your doctor may recommend that you learn to insert a soft tube (catheter) into your urethra several times a day to drain your bladder. You’ll be instructed on how to clean these catheters for safe reuse.
- Prevention is better than cure: Healthy lifestyles and avoiding excessive intake of caffeine and alcohol are recommended.
Conclusion:
Due to the embarrassment induced or invoked, patients report urinary incontinence only when it is severe and hinders regular social activities. Early reporting to a doctor with the slightest experience of discomfort is therefore necessary.
It is not embarrassing,
It is just social stereotypes trespassing,
Just a pinch of scientific reliance,
Can get the bladder back to voluntary compliance…
Illustration by: Dribble
Author


1 thought on “Everything you should know about Urinary Incontinence”
This is such an informative and well-written article on urinary incontinence. I think it’s so important to educate people about this condition, as it affects so many individuals but often goes undiscussed. The article covers all the important aspects, from treatment and symptoms of urinary incontinence, and does so in a compassionate and understanding way.